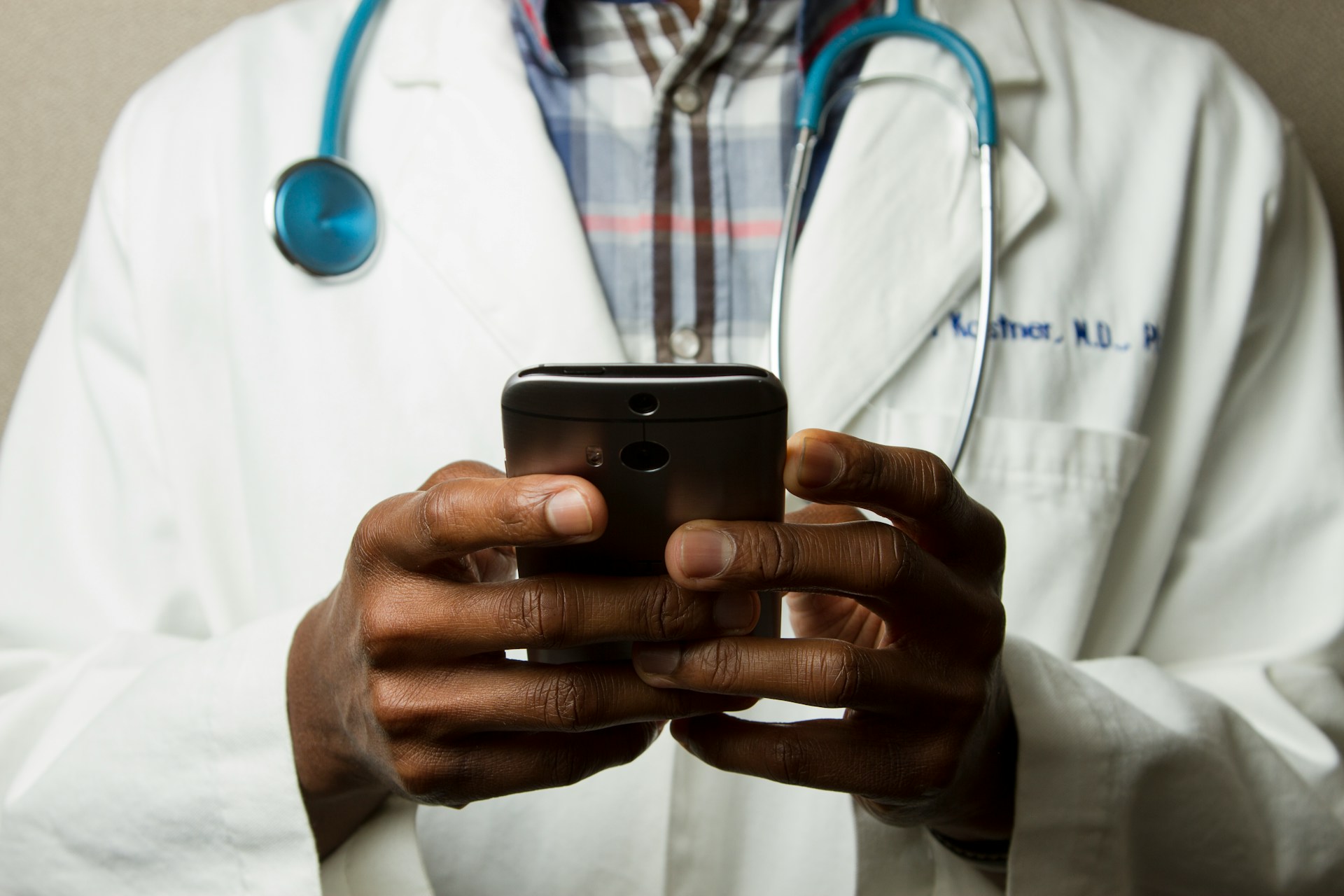
Discover how healthcare providers adapt to telehealth, balancing efficiency and personal connection, while tackling technology and training challenges.
Virtual care is no longer optional. It’s changed how many providers give care and how they spend their day. Three out of four physicians now use telehealth regularly—a major shift from five years ago. Some gain efficiency. Others lose personal connection. Speed comes at a cost; these tools are hard on us. They allow more access, but extend work hours. The balance is not always clear. Every speciality responds differently. However, remember this: This is a lasting change; it’s not going away. Providers are adapting fast, often without support. Systems are evolving at a fast rate; however, human adaptation needs to improve to keep up. Think of it like this: the car is faster, but the driver needs more training.
Healthcare Provider Perspectives On Virtual Care
Healthcare providers have seen their daily practice altered radically due to virtual care. A 2023 survey showed that 74.4% of physicians offer telehealth services in their practices, almost triple the numbers from 2018. This major change is a double-edged sword for healthcare; it offers amazing potential, but also throws up some significant obstacles. Doctors will need to adapt.
Efficiency And Time Management
Doctors say telehealth has improved their clinical output. Virtual visits usually take about 12 minutes. 20% less time than seeing patients in person. Less paperwork means more time for patients; doctors can help more people.
“Telehealth takes down the boundaries of clinic,” one physician said, noting how virtual care blends work and personal life. The accessibility works both ways. While 83% of doctors want virtual care as a permanent option, easy access often means longer workdays.
Different specialities use telehealth at varying rates:
- 83.1% of psychiatrists provided video visits in a recent week
- 66.8% of primary care physicians
- 64.3% of medical specialists
- 45.3% of surgeons
Doctors value telehealth’s role in managing chronic conditions. 54.9% of physicians used telehealth to monitor ongoing diseases in 2022, a dramatic rise from 9.9% in 2018.
Challenges In Building Rapport
Screen-based connections create unique challenges. One provider mentioned that not being “there physically for a patient is extraordinarily difficult”. Medical professionals consistently say rapport makes or breaks telehealth interactions.
Patients sometimes notice their doctors getting distracted during video visits: “I’m staring at her in her house and her cat’s walking by and every once in a while, her eyes dart away”. Others think telehealth video conferencing creates “more of a direct connection because providers have no distractions”.
New patient relationships prove harder to build online. One provider said, “It’s just very different from being in a room with somebody”. Yet, existing relationships often grow stronger online, and some patients feel more connected than they did during in-person visits.
Training And Adaptation To New Tools
The pandemic left no choice, 85% of physicians learned virtual care in under two weeks, while 43% received no help at all. We learned a hard lesson: Proper training is essential. Sink or swim, it made all the difference.
Medical facilities now recognize several vital telehealth roles:
- Telehealth Champions who lead program implementation
- Program Managers overseeing daily logistics
- Education Managers ensuring staff training
- Device Managers handling technical aspects
Modern training programs teach digital communication skills. Providers learn to interview patients online and spot subtle cues despite technology barriers. Cultural humility training helps curb stigma about traditionally underserved communities.
Office space setup makes a difference. Quiet, well-lit areas improve patient experience. Most clinics weren’t built with telehealth in mind, so finding quiet spaces remains a challenge for providers.
Technology And Infrastructure Requirements
Telehealth success relies on strong technical foundations. A well-built infrastructure connects patients with providers and powers those smooth virtual doctor visits.
Internet Speed And Device Compatibility
Reliable internet connectivity serves as the foundation of telehealth programs. Patients need minimum speeds of 10 Mbps download and 5 Mbps upload for simple video consultations. Fast speeds prevent interruptions during important doctor talks.
Healthcare facilities need varying bandwidth based on their size:
- Single physician practices: 4 Mbps minimum
- Small practices (2-4 physicians): 10 Mbps
- Clinics (5-25 physicians): 25 Mbps
- Hospitals: 100 Mbps
- Large medical centres: 1,000 Mbps
Device requirements remain straightforward. Patients can use a smartphone, tablet, or computer with internet access. Public locations like libraries offer wireless connections for private virtual visits when patients lack home internet.
“Think of your device as the front door to telehealth,” explains Dr. Maria Chen. “Almost any internet-connected gadget with a camera works nowadays.”
Security And HIPAA Compliance
Patient privacy protection stands as a crucial part of telehealth technology. HIPAA Rules apply to all covered health care providers offering telehealth services.
FaceTime and Skype apps don’t meet HIPAA compliance standards by default. Healthcare organizations must partner with technology vendors that sign HIPAA business associate agreements.
The temporary relaxation of telehealth HIPAA enforcement ended after a 90-day transition period following the COVID-19 emergency period on May 11, 2023. A provider’s success hinges on meeting specific criteria; for example, licensing, insurance, and background checks.
- Encrypted technology implementation
- Virtual private network (VPN) utilization
- Strong authentication parameters
- Regular security testing
Integration With EHR Systems
A unified patient care environment emerges when telehealth platforms connect with electronic health record systems. US hospitals’ certified EHR platform usage exceeds 95%, which makes integration vital.
EHR integration helps maximize telehealth benefits, as providers already know the baseline system. This connection allows immediate access to patient data during telehealth video conferencing API.
The way things are in many hospitals is that doctors use one system, the labs use another, and patient monitoring is yet another system. This is inefficient. Data sharing becomes vulnerable to security threats due to these technical incompatibilities. On top of that, it creates clerical burdens that lead to physician burnout when systems don’t work well together.
Well-executed integration delivers clear benefits: quick information updates after remote visits, better patient participation, and improved follow-up care.
Conclusion
Telehealth has opened doors—and exposed weak spots. It improves time use but challenges relationships. It connects rural patients while placing new burdens on providers. Behind every video call are real infrastructure demands and complex tech requirements. Successful use depends on training, tools, and fast systems that don’t break under pressure. Integration with EHRs still lags in many places. Security rules remain strict, as they should. Doctors are adjusting. Some thrive. Others struggle. The path ahead isn’t simple, but it’s clear. Telehealth isn’t a temporary solution. It’s a permanent shift in how modern care gets done. Providers just want it to work.
Was this news helpful?




 Yes, great stuff!
Yes, great stuff! I’m not sure
I’m not sure No, doesn’t relate
No, doesn’t relate



